Setting up a pharmaceutical cleanroom is one of the most critical activities in the pharmaceutical industry. A cleanroom is not merely a controlled space, but it is a scientifically designed and highly regulated environment intended to minimize contamination risks. Any gaps in planning, design, or execution can result in deviations, regulatory observations, product recalls, or even shutdown of operations.
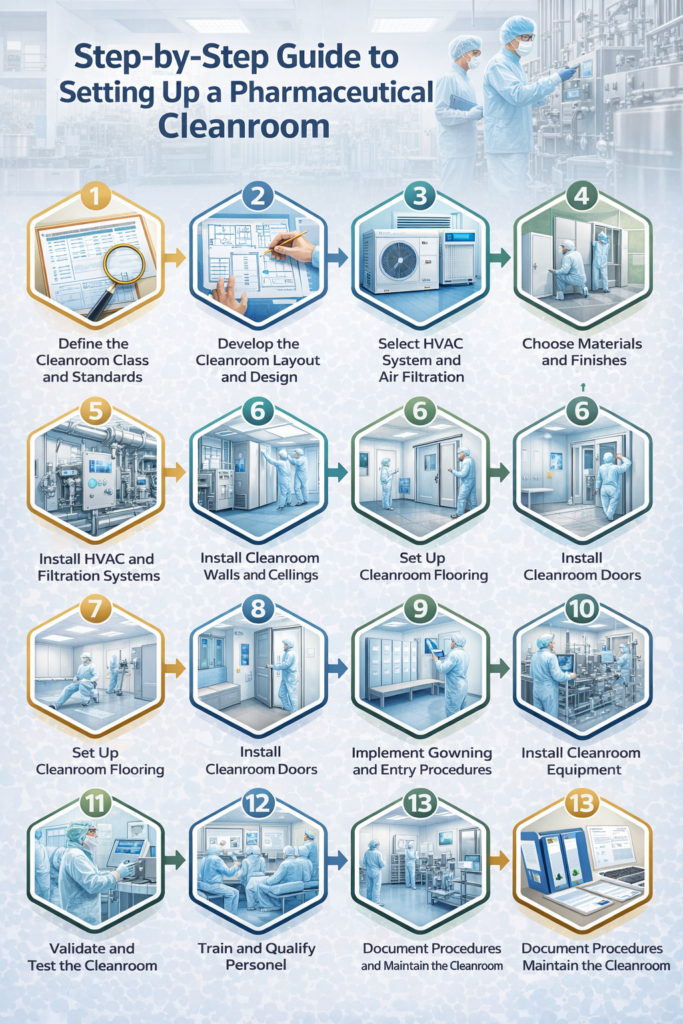
This step-by-step guide explains the entire cleanroom setup process, starting from conceptual planning and ending with regulatory readiness.
Step 1: Define the Product, Process, and Regulatory Requirements
The foundation of a cleanroom project begins with a clear understanding of the product and the manufacturing process. At this stage, organizations must define what type of pharmaceutical product will be manufactured, such as sterile injectables, oral solid dosage forms, ophthalmic preparations, biologics, or APIs. The nature of the process, whether it involves aseptic filling, terminal sterilization, granulation, coating, or packaging, directly influences cleanroom design.
Equally important is identifying the target markets for product distribution. Regulatory expectations vary between regions such as India, the United States, Europe, and WHO-regulated markets. Each authority has specific GMP requirements that impact cleanroom classification, monitoring, and documentation.
This step is critical because different products demand different environmental controls. For example, aseptic manufacturing requires high-grade cleanrooms, while non-sterile operations may function under controlled but less stringent conditions. The outcome of this step is a clear definition of cleanroom grades, regulatory expectations, and overall contamination control needs.
Step 2: Perform Risk Assessment and Contamination Control Strategy (CCS)
After defining the product and regulatory expectations, the next step is to perform a systematic risk assessment. Design the pharmaceutical cleanrooms using a risk-based approach to identify and control potential sources of contamination. These sources commonly include personnel, materials, equipment, air, and surfaces.
Risk assessment tools such as Failure Mode and Effects Analysis (FMEA) or Hazard Analysis and Critical Control Points (HACCP) are used to evaluate where contamination could occur and how severe the impact might be. Based on this assessment, appropriate control measures are identified.
Modern GMP regulations, particularly EU GMP Annex 1, require the preparation of a comprehensive Contamination Control Strategy. This document explains how to control contamination risks through facility design, HVAC systems, personnel and material flow, cleaning and disinfection practices, and environmental monitoring. The outcome of this step is a documented CCS that serves as a guiding framework for all subsequent design and engineering decisions.
Step 3: Cleanroom Layout and Facility Design
After understanding the risks, the next phase involves designing the cleanroom layout. Facility design must support smooth operations while minimizing contamination risks. The layout should ensure a logical and unidirectional flow of personnel, materials, and waste, avoiding cross-contamination and backtracking.
Pharmaceutical cleanrooms typically include change rooms, airlocks, manufacturing areas, corridors, and technical service spaces. Apply zoning concepts such as black, grey, and white areas to gradually transition from uncontrolled to highly controlled environments.
Proper segregation of activities, pressure cascades between rooms, and well-defined movement pathways are essential elements of a GMP-compliant design.
Step 4: Define Cleanroom Classification and Environmental Conditions
Each room within the facility must be assigned a cleanroom classification (Grade A, B, C, and D) based on its intended use and risk level. Cleanroom grades define acceptable particle concentrations and microbial limits under both at-rest and in-operation conditions.
In addition to classification, environmental parameters such as temperature, relative humidity, and differential pressure must be specified. These conditions help ensure product stability, operator comfort, and contamination control. Cleanrooms operate within defined temperature and humidity ranges, with pressure differentials maintained to prevent ingress of contaminants.
The outcome of this step is a documented set of room-wise environmental specifications that guide HVAC design and qualification activities.
Step 5: HVAC System Design and Engineering
The HVAC system is considered the heart of a pharmaceutical cleanroom.
It is responsible for controlling airborne contamination, maintaining cleanroom classification, and providing a comfortable working environment for personnel.
HVAC design includes the selection of HEPA filters, determination of air change rates, airflow patterns, and pressure cascades. Depending on the process, airflow may be unidirectional or turbulent. Properly designed HVAC systems ensure continuous dilution and removal of particles and microorganisms.
At this stage, prepare detailed engineering documents such as airflow diagrams, pressure cascade drawings, and HVAC design qualification protocols.
The outcome is an HVAC system design capable of consistently maintaining required cleanroom conditions.
Step 6: Selection of Cleanroom Construction Materials
Materials used in cleanroom construction play a vital role in maintaining cleanliness and durability.
All surfaces must be smooth, non-shedding, and resistant to water and chemicals.
Walls, ceilings, floors, doors, and windows are selected based on their cleanability and compatibility with disinfectants. Flooring systems often include epoxy or polyurethane coatings with coved joints to eliminate corners where contaminants could accumulate.
Step 7: Utilities and Support Systems Planning
Cleanroom operations depend heavily on clean and reliable utilities. These include purified water or water for injection, clean steam, compressed air, nitrogen, electrical systems, and backup power supplies.
Utilities must be designed to avoid dead legs, ensure proper drainage, and allow easy access for maintenance. Clear labeling and flow direction markings are essential to meet GMP expectations. The outcome of this step is a robust utility infrastructure that supports uninterrupted and compliant operations.
Step 8: Equipment Selection and Placement
Process equipment must be compatible with cleanroom conditions and aligned with the manufacturing process. Equipment surfaces should be smooth and easy to clean, with adequate space provided for operation, cleaning, and maintenance.
During this phase, supplier qualification, factory acceptance testing, and site acceptance testing are planned to ensure the equipment meets GMP and performance requirements. The outcome is properly selected and positioned equipment that integrates seamlessly into the cleanroom environment.
Step 9: Installation, Construction, and Execution
This phase involves translating approved designs into a physical facility. Cleanroom panels, HVAC systems, utilities, and equipment are installed according to qualified drawings and specifications.
Carefully control the construction activities prevent damage. After installation, thorough cleaning is performed, and all work is documented. The outcome of this step is a physically complete cleanroom ready for qualification activities.
Step 10: Cleanroom Qualification (DQ, IQ, OQ, PQ)
Qualification demonstrates that the cleanroom is designed, installed, and operating as intended.
Design Qualification confirms compliance with GMP requirements, while Installation Qualification verifies correct installation.
Operational Qualification tests system performance under defined conditions, and Performance Qualification confirms consistent performance during routine operations.
Tests include airflow visualization, HEPA filter integrity testing, viable and non-viable particle counts, and recovery time studies.
The outcome is a fully qualified cleanroom that meets regulatory expectations.
Step 11: Cleaning, Disinfection, and Environmental Monitoring Setup
Once qualification is complete, cleaning and disinfection programs are implemented.
These programs define cleaning agents, disinfectant rotation, frequencies, and methods based on risk assessment.
Establish environmental monitoring systems to routinely assess air, surface, and personnel contamination levels.
Define alert and action limits, and trending mechanisms are implemented to detect early signs of contamination.
The outcome is a controlled environment continuously monitored for compliance.
Step 12: Personnel Training and Gowning Qualification
Personnel are the largest source of contamination in cleanrooms. This makes training essential. Operators are trained in GMP principles, cleanroom behavior, gowning procedures, and aseptic techniques.
Initial qualification and periodic requalification ensure that personnel maintain required standards.
For aseptic areas, participation in media fill studies further demonstrates operator competence.
The outcome is a trained workforce capable of working safely and compliantly within cleanroom environments.
Step 13: Regulatory Readiness and Continuous Improvement
Before commercial production begins, the facility must be prepared for regulatory inspections. This includes ensuring documentation completeness, SOP implementation, and successful internal audits.
Cleanroom performance must be continuously reviewed through environmental monitoring trends, deviation analysis, and periodic system upgrades.
Regulatory guidelines evolve over time, and cleanrooms must adapt accordingly.
The outcome of this step is an inspection-ready facility with a culture of continuous improvement.
Setting up a pharmaceutical cleanroom is a structured, risk-based, and highly regulated process. When each step is executed in the correct sequence, the facility will consistently meet the cleanroom requirements.
For pharmaceutical professionals, understanding this process is essential not only for building cleanrooms but also for maintaining them throughout their lifecycle. A well-designed and well-managed cleanroom ultimately protects patients, products, and the organization’s regulatory standing.




